If you’re suffering from jaw pain, clicking, or discomfort in your jaw joint, you might be searching for TMJ treatment Calgary options. At South Calgary Oral Surgery, our team of specialists offers a range of solutions for temporomandibular joint (TMJ) disorders, designed to help you find lasting relief. TMJ disorders can severely affect your ability to eat, speak, or even yawn without pain, but you don’t have to live with it.
We’ll explore the three primary treatment options we offer: Botox injections, TMJ arthrocentesis, and open joint surgery, and how they work to alleviate TMJ pain and restore function.
Understanding TMJ Disorders

The temporomandibular joint is one of the most used joints in the body. Located on both sides of your head, it connects your jawbone to your skull, allowing you to chew, talk, and yawn. When this joint becomes overworked or inflamed, you can experience painful symptoms such as pain, limited movement, or a clicking noise—common symptoms of TMJ disorder.
TMJ treatment Calgary often begins with identifying the severity of the disorder and choosing the best approach. At South Calgary Oral Surgery, we offer personalized treatment plans based on the needs of each patient. Let’s take a closer look at the TMJ treatments available at our practice.
Botox for TMJ: A Minimally Invasive Solution for TMJ Pain Relief

One of the innovative treatments we offer for TMJ treatment Calgary is Botox injections. Botox is well-known for cosmetic uses, but it’s also effective for reducing muscle tension in the jaw associated with TMJ disorders. When injected into the facial muscles, Botox temporarily relaxes them, reducing the grinding or clenching that causes jaw pain.
This procedure is quick and done in-office, typically lasting between 10 to 30 minutes. Many patients find that Botox helps relieve their jaw pain and discomfort after just a few days. The effects generally last for several months, and the procedure can be repeated as needed.
Benefits of Botox for TMJ
Relaxes the overworked muscles causing pain
Minimally invasive with little downtime
Can be combined with other TMJ treatments for optimal results
Patients who undergo Botox for TMJ treatment in our Calgary clinic report reduced pain and improved jaw function, allowing them to return to daily activities with ease. While there may be mild side effects like temporary bruising or numbness, Botox is generally safe and effective for most people.
TMJ Arthrocentesis: Flushing Away the Pain

When conservative treatments like Botox aren’t enough, TMJ arthrocentesis offers a more hands-on approach to TMJ treatment, particularly for those suffering from facial pain. This procedure is ideal for patients with joint inflammation or fluid buildup that’s causing discomfort. Arthrocentesis involves flushing the temporomandibular joint to remove excess fluid and reduce inflammation.
During this procedure, a small needle is inserted into the joint space, and sterile fluid is used to wash out debris and inflammatory by-products within the joint. Often, a steroid is injected into the joint at the end of the procedure to further reduce swelling and promote healing.
TMJ treatment Calgary patients who choose arthrocentesis often experience significant relief from symptoms. The procedure is typically performed under general anesthesia, so you’ll be asleep and comfortable during the process.
Why Choose Arthrocentesis?
Effective for reducing TMJ pain and inflammation
Minimal recovery time
Can be performed if conservative therapies fail
If you’re struggling with persistent jaw pain, arthrocentesis may be the solution you need to restore comfort and functionality to your jaw.
Open Joint Surgery: A Comprehensive Solution for Severe TMJ Disorders and Jaw Joints

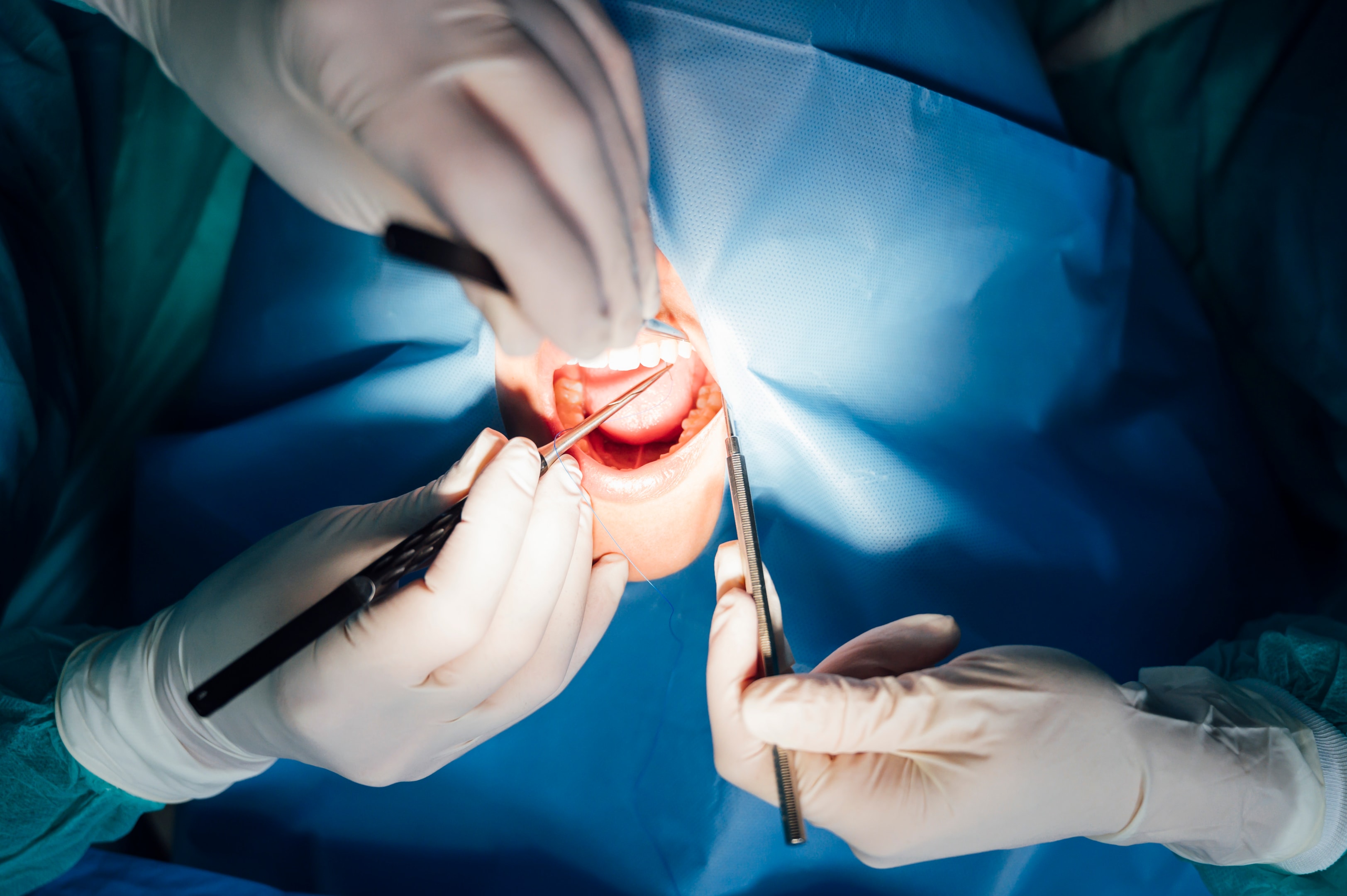
For more advanced or severe TMJ disorders, open joint surgery may be necessary. This option is reserved for cases where other TMJ treatments have not provided adequate relief, or the joint is severely damaged. In this procedure, the surgeon makes an incision near the joint to gain access and directly address the underlying issue, whether it’s a misaligned disc, scar tissue, or bone fragments.
Unlike less invasive treatments, open joint surgery requires a longer recovery period, but the results can be life-changing for patients with advanced TMJ issues. During your consultation, your surgeon will explain the specific approach for your case and discuss the risks and benefits involved.
When to Consider Open Joint Surgery:
Severe joint damage, such as bone chips or tumors
The joint has fused together (ankylosis)
Arthrocentesis and Botox have not been successful
Although it’s a more extensive treatment option, open joint surgery offers long-lasting relief for patients whose TMJ disorders are significantly affecting their quality of life.
TMJ Symptoms and Causes
TMJ symptoms can vary widely from person to person, making it essential to understand the common causes of temporomandibular joint disorder (TMJ). Here are some of the primary factors that can lead to TMJ pain:
Jaw Misalignment: When your jaw is not properly aligned, it can put undue strain on the temporomandibular joint, leading to pain and discomfort. This misalignment can affect the way your teeth fit together and how your jaw moves.
Bruxism: Grinding or clenching your teeth, often unconsciously, can cause significant tension in the jaw muscles. This constant pressure can lead to TMJ pain and exacerbate existing issues.
Stress and Anxiety: High levels of stress and anxiety can manifest physically, causing tension in the facial muscles. This tension can contribute to TMJ symptoms, making it important to manage stress effectively.
Jaw or Facial Injuries: Trauma to the jaw or face, such as from an accident or sports injury, can result in TMJ pain and discomfort. These injuries can damage the jaw joints and surrounding tissues.
Arthritis: Certain types of arthritis, like osteoarthritis, can cause inflammation and pain in the temporomandibular joint. This inflammation can lead to chronic TMJ symptoms and require specialized treatment.
Understanding these causes can help you identify potential triggers for your TMJ pain and seek appropriate treatment.
Diagnosing TMJ Pain

Diagnosing TMJ pain involves a comprehensive approach that includes a physical examination, medical history review, and diagnostic tests. Here’s what you can expect during the diagnostic process:
Physical Examination: Your oral surgeon will conduct a thorough examination of your jaw, face, and head. They will check for tenderness, clicking, or popping sounds in the jaw joints.
Medical History: A detailed review of your medical history can help identify any underlying conditions that may be contributing to your TMJ disorder. This includes discussing any past jaw or facial injuries or habits like teeth grinding.
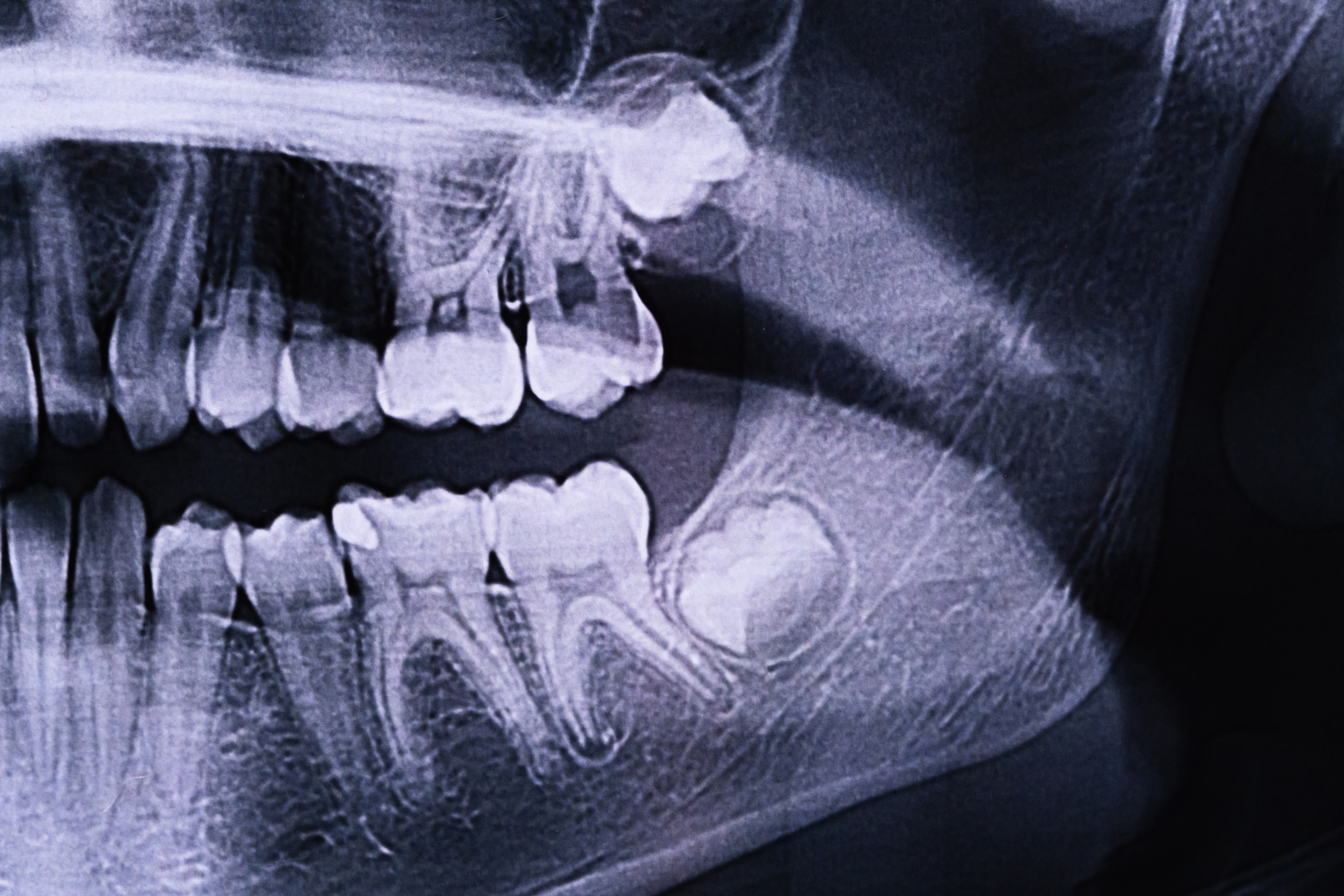
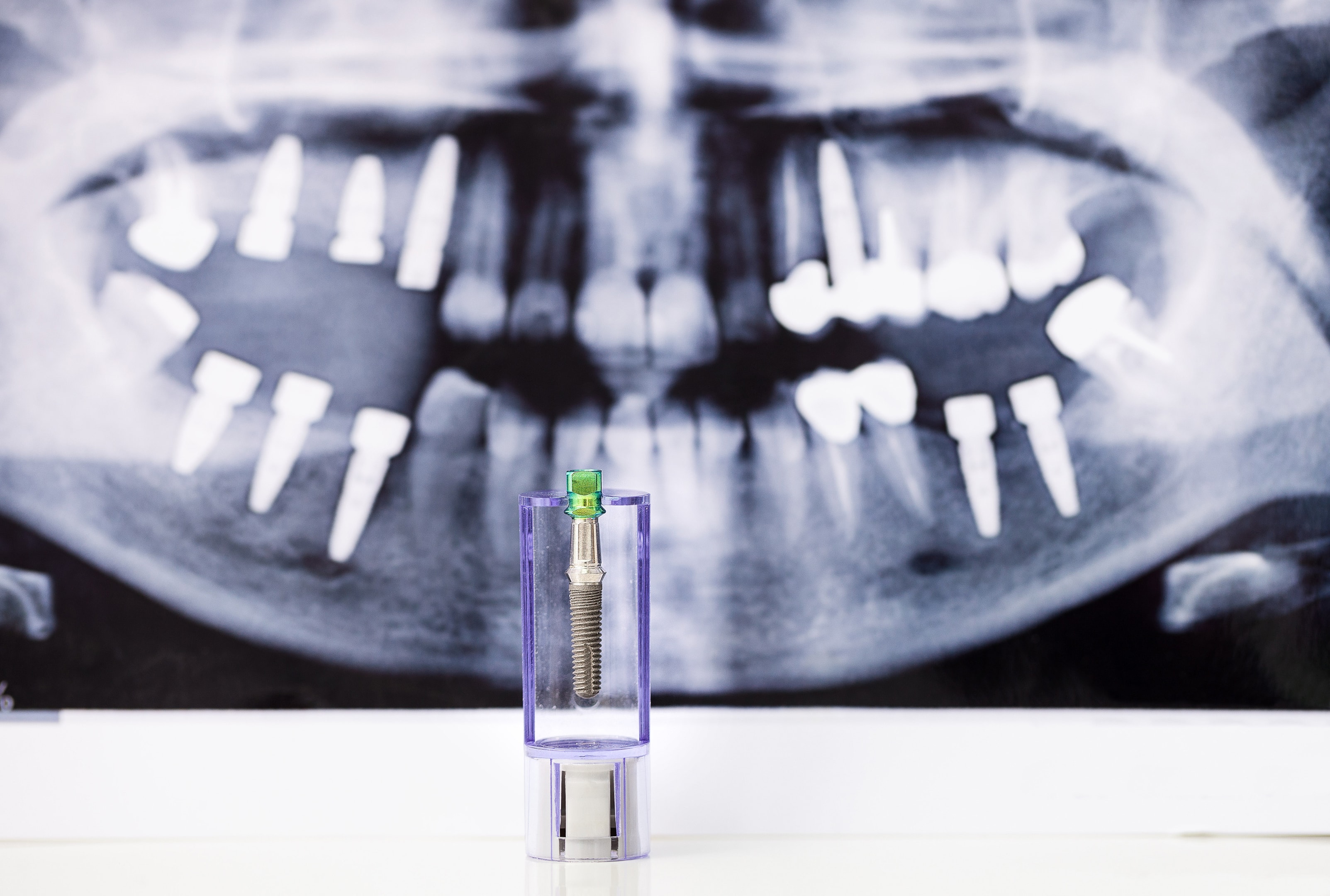
X-rays: X-rays are often taken to evaluate the alignment of your jaw and the condition of the temporomandibular joint. This imaging helps in identifying any structural issues.
CT or MRI Scans: For a more detailed view, CT or MRI scans may be used to assess the soft tissues and bones of your jaw and face. These scans can reveal issues that X-rays might miss.
Bite Analysis: A bite analysis can help evaluate the alignment of your teeth and how they fit together. This can be crucial in identifying jaw misalignment that may be causing TMJ pain.
It’s important to seek medical attention if you are experiencing persistent or severe TMJ pain, as untreated TMJ disorders can lead to further complications, such as:
Chronic Pain: Persistent TMJ pain can become chronic, leading to ongoing discomfort and affecting your quality of life.
Tooth Wear: Grinding or clenching your teeth can cause significant wear and tear, leading to tooth decay and sensitivity.
Headaches and Ear Pain: TMJ pain can radiate to your head and ears, causing frequent headaches and ear pain.
Shoulder Pain: The discomfort from TMJ pain can also extend to your shoulders, causing stiffness and additional pain.
An oral surgeon or healthcare professional can offer TMJ pain relief through a variety of treatments, including:
TMJ Treatments: Customized treatments, such as mouth guards or splints, can help alleviate TMJ pain and discomfort by reducing strain on the jaw muscles.
Pain Relief Medications: Medications like pain relievers or muscle relaxants can help manage TMJ pain effectively.
Physical Therapy: Physical therapy techniques, such as massage or specific exercises, can help relax the jaw muscles and improve range of motion.
Lifestyle Changes: Implementing lifestyle changes, such as stress management techniques or dietary adjustments, can help manage TMJ pain and prevent further complications.
By understanding the diagnostic process and available treatments, you can take proactive steps towards finding relief from your TMJ pain.
What to Expect from TMJ Treatment at South Calgary Oral Surgery
When you choose South Calgary Oral Surgery for TMJ treatment Calgary, you can expect a team of compassionate experts dedicated to your well-being. We offer individualized care to every patient, ensuring that the most appropriate treatment plan is selected for your specific condition.
Botox injections for muscle tension relief
TMJ arthrocentesis to reduce inflammation and discomfort
Open joint surgery for complex cases requiring structural repair
Our goal is to provide effective, lasting solutions for your TMJ disorder, so you can return to your normal activities without pain or discomfort. We understand that every patient’s journey is different, and we’re here to support you at every step.
How TMJ Treatment in Calgary Can Improve Your Quality of Life

Living with TMJ pain can be incredibly challenging. From difficulty chewing to chronic headaches, the symptoms can interfere with everyday life. Fortunately, with the right TMJ treatment Calgary, you don’t have to continue suffering.
Whether you’re a candidate for Botox, arthrocentesis, or open joint surgery, our team at South Calgary Oral Surgery is here to help you reclaim comfort and function in your jaw.
Ready to Learn More About Your TMJ Treatment Options?
If you’re experiencing jaw pain or discomfort, don’t wait to seek professional help. At South Calgary Oral Surgery, we specialize in TMJ treatment Calgary patients can trust. Contact our office today to schedule a consultation and discuss which treatment is right for you. Let us help you take the first step toward a pain-free future!